We're here to help
Please refer to the guidelines on this page before making a referral to VNH. If you have any questions, please call the Intake team at 888-300-8853, Option 1. We are here to assist you and help make the referral process go as smoothly as possible.
Make a referral
Epic
Providers can refer patients for VNH services seamlessly within Epic. Benefits include:
- Streamlined referral process
- Direct access to patient notes from the VNH staff caring for your patients
- Streamlined communication using the in-basket messaging system within Epic
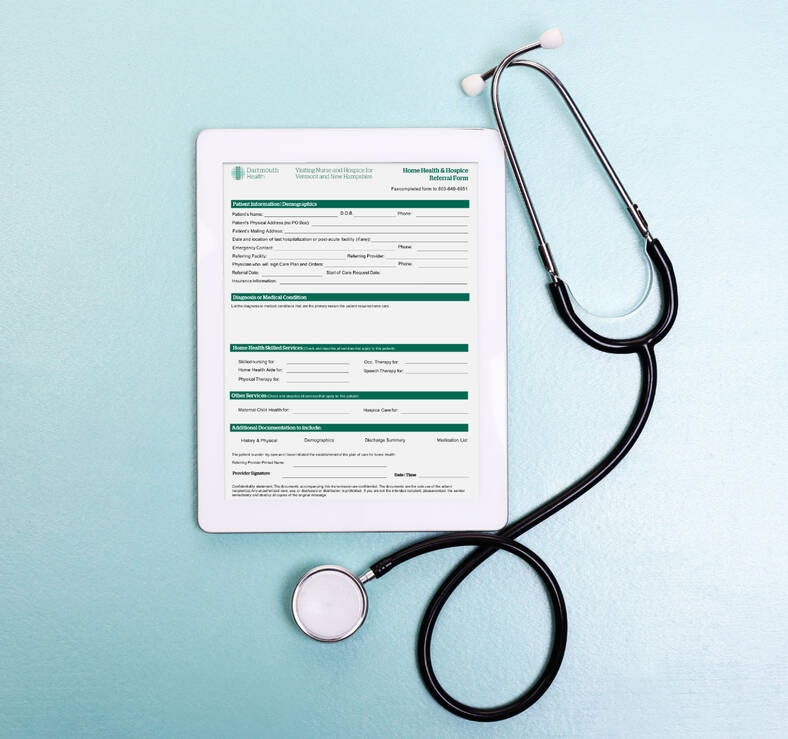
Fax
Providers using other Electronic Medical Records can refer patients for VNH services by completing the Home Health & Hospice Referral Form and faxing it to 603-640-6851.
We also accept referrals via Wellsky, CarePort and AIDA Healthcare.
Home health care referral guidelines
Medicare requires that a patient have a skilled need and be homebound. Most other insurances have similar requirements for adult home health care. A skilled need is medically necessary care that can only be delivered under the direction of a skilled or licensed clinician.
Examples of need
Nursing
- Observation and assessment of the patient’s condition when there is a reasonable potential for change in condition
- Teaching and training activities
- Patients with wounds with family to be providing wound care as taught by the nurse
- Tube feedings
- Administration of some injectable medications
- Catheters
- Wound care
- Ostomy care
- Bowel and bladder training programs
Physical Therapy
- Teaching safety awareness when ambulating and transferring to reduce fall risk
- Providing pain interventions using modalities or corrected movements
- Evaluating the home environment and suggesting modifications to improve safety
- Recommending and instructing the use of assistive devices
- Identifying gait deviations and retraining poor patterns
- Addressing complications of dizziness or lack of balance
- Developing exercise programs to improve strength and range of motion
- Educate caregivers on maintaining patient safety in the home
- Simple wound care
Occupational Therapy
- Teaching safety awareness when ambulating and transferring to reduce fall risk
- Providing pain interventions using modalities or corrected movements
- Evaluating home environment and suggesting modifications to improve safety
- Recommending and instructing the use of assistive devices
- Identifying gait deviations and retraining poor patterns
- Addressing complications of dizziness or lack of balance
- Developing exercise programs to improve strength and range of motion
- Educate caregivers on maintaining patient safety in the home
- Simple wound care
Speech Language Pathology
- Assess and treat swallowing impairment (dysphagia)
- Assess and treat voice disorders (aphasia, dysphasia, dysarthria, etc.)
- Assist patients to communicate both verbally and non-verbally
- Complete comprehensive cognition assessments and treat with structured memory and problem-solving tasks
Homebound definition
Requires a taxing effort because of illness or injury and may include the use of a supportive device (i.e. walker, cane, wheelchair, special transportation, etc.)
- Is medically contraindicated due to a specific condition
- Is infrequent, or of short duration for healthcare purposes. (Additional infrequent absences for a short duration may not indicate that the patient is not homebound and can be discussed with the VNH care team)
The following are some (but not all) examples of situations that may render a patient homebound.
- Vision impairment
- Cognitive impairment/dementia
- Cardiac or pulmonary disease, causing fatigue and shortness of breath
- Post-op patients on pain medications
- Inability to bend and twist as required to enter/exit car
- Bedbound or wheelchair-bound
- Paralysis or hemiparesis
- Inability to open doors or use handrails
- Activity restrictions
Face-to-face requirement
Medicare requires documentation of a completed, valid, and signed face-to-face encounter for a patient to be eligible for home health services. The face-to-face encounter is a Medicare requirement; however, most insurances have followed Medicare and also require a valid face-to-face. The encounter must be completed by a PECOS enrolled physician or other approved non-physician practitioner, which can include nurse practitioners, clinical nurse specialists, and physician assistants. The face-to-face encounter must be performed by the provider following the patient during the home health episode unless a patient is referred directly from an inpatient facility.
Required components of a face-to-face encounter document:
- A clinical note performed and signed and dated by an allowed provider type. A handwritten signature must have a handwritten date and an electronic signature and date must be clearly identified as being an electronic signature. If the encounter is performed by a resident, the encounter note must be co-signed by the supervising attending who will follow the patient during the home health episode.
- Encounter may be up to 90 days prior to the home health start of care or may take place within 30 days after the start of care.
- The encounter must be related to the reason for the referral and admission to home health. The not must include the clinical diagnosis, assessment and plan for the treatment of the issue.
- The encounter or related documentation from the facility or provider must include documentation supporting that the patient is homebound.
Valid face-to-face encounter documentation can be found in an office visit note, progress note, emergency department notes and discharge summaries. Please note that not all discharge summaries include a valid assessment/clinical findings. If it only includes patient instructions, medication list, nursing or therapy notes, it is not a valid face-to-face.
Please reach out to the Intake team at 800-300-8853, Option 1 with any questions related to the face-to-face documentation. We are here to assist you and help make the referral process go as smoothly as possible.
Valid reimbursable diagnoses
Medicare reimbursement is determined based on the patient’s diagnoses. The primary diagnosis must be as specific as possible and there are a number of diagnoses that are excluded from payment. Many of these excluded diagnoses are unspecified diagnoses or symptoms, such as weakness, debility, abnormal gait, dizziness, and fatigue. They can also include diagnoses that do not specify whether the injury, surgery or wound is on the right or left side of the body.
The home health primary diagnosis should reflect the underlying cause for the patient symptoms and be as specific as possible. Some examples may include:
Muscle weakness, Generalized weakness
Consider: What is the reason the patient is presenting with muscle weakness? Did the patient have surgery, an injury, cardiac or respiratory condition? Did the patient have an infection? Identify what caused the weakness.
Debility
Same as weakness guidance. Old age is not a valid diagnosis under PDGM.
Abnormal gait
What is the abnormal gait related to? Is there an underlying neurological cause? Even variations of abnormal gait such as ataxic gait, difficulty in walking, etc. are not allowed as a primary diagnosis by Medicare.
Superficial injury codes
Superficial injury codes, most used to capture skin tears and abrasions, are NOT allowed as a valid primary diagnosis by Medicare. Consider a laceration code, if more appropriate. Why did the patient receive a skin tear? Falling? Loss of balance? Identify the cause rather than the symptoms.
Please reach out to the Intake team at 800-300-8853, Option 1 with any questions related to the appropriate diagnosis. We are here to assist you and help make the referral process go as smoothly as possible.
Hospice care referral guidelines
The decision to enter hospice is a difficult one for patients, their caregivers, and their providers. Patients receiving hospice services from VNH benefit from:
- Dedicated hospice RN who coordinates with the entire hospice team
- Emotional and spiritual support for patients and their caregivers
- 24/7 phone support for changes in clinical status and after-hours home visits for difficult situations
- Expert pain and symptom management guided by our hospice-certified medical director
- Shared medical record with DH primary care providers, specialists and VNH's hospice care team
Providers utilizing hospice services from VNH benefit from:
- Clinical assessments and progress reports
- Decrease in patient/family crisis calls
- Support of hospice Medical Director
- Availability of office co-visit by hospice nurse to assist with patient education and end-of-life decision making
- Primary physician remains a member of the hospice team
Hospice can be appropriate for patients with either a cancer or non-cancer diagnosis. Admission to hospice requires a clinical judgment that a patient's prognosis is less than six months should the disease follow its normal trajectory. Non-cancer illnesses tend to be unpredictable and characterized by fluctuations in both symptoms and their severity, making hospice diagnosis more difficult. However, patients do benefit most from early referrals to a hospice program.
Patients with the following conditions may be appropriate for hospice:
General Guidelines
Life limiting condition
Progression of disease
Frequent hospitalization, office and/or emergency room visits
Weigh loss >10% over past six months
Serum albumin <2.5dl
Patient/family focus on symptom relief, not cure
End-Stage Pulmonary Disease
Dyspnea at rest
FEV1 <30% after bronchodilators
Recurrent pulmonary infections
Cor pulmonale/right heart failure
p02 < 55mm HG or 02 sat <88% (on oxygen)
Persistent resting tachycardia
Cardiogenic embolic disease (e.g. CVA)
Weight loss > 10% over past six months
End-Stage Renal Disease
Patient not seeking dialysis or transplant
Creatinine clearance < 10cc/min (<15cc/min for diabetics)
Creatinine >8mg/dl (>6mg/dl for diabetics)
Symptoms of uremia (confusion, nausea/vomiting, pericarditis)
Hyperkalemia >7.0 mEq/L
Oliguria <400cc/24 hours
End-Stage Cardiac Disease
Symptomatic despite optimal treatment with diuretics and vasodilators
Recurrent CHF, NYHA Class III or Class IV
Ejection fraction <20%
Arrhythmias are resistant to treatment
History of cardiac arrest or resuscitation
Cardiogenic embolic disease (e.g. CVA)
Angina at rest
Persistent resting tachycardia
End-Stage Liver Disease
Patient is not a candidate for a liver transplant
PTT > 4 seconds over control
Serum albumin < 2.5 gm/dl
Ascites refractory to treatment
Peritonitis
Hepatic encephalopathy, refractory to treatment
Hepatorenal syndrome
Progressive malnutrition
Continued active alcoholism
End-Stage Dementia
Functional Assessment Staging Tool (FAST) score >7
Unable to ambulate without assistance
Unable to dress or bathe without assistance
Bowel and bladder incontinence, intermittent or constant
No meaningful verbal communications
Complications such as aspiration pneumonia, UTI, septicemia, recurrent fevers
Pressure Injury Stage 3 or 4
Weight loss of 10% over last six months
Stroke and Coma
Coma or persistent vegetative state > 3 days
Dysphagia without artificial nutrition and/or hydration
Dependence in all ADLs
Post-stroke dementia
Bowel and bladder incontinence
Family wants palliative care
Absent verbal response
End-Stage Neurological Diseases (ALS)
Wheelchair or bed-bound
Barely intelligible speech
Difficulty swallowing
Nutritional status declining
Needs major assist in all ADLs
Dyspnea at rest and requires oxygen
Declines assisted ventilation
Patients with a Cancer Diagnosis
Disease with metastases at presentation or progression from an earlier stage of the disease to metastatic disease with EITHER continued decline in spite of further disease-related therapy OR patient declines further disease-related therapy.
Certain cancers with poor prognosis–small cell lung cancer, brain cancer and pancreatic cancer–may be hospice eligible without fulfilling the other criteria in this section.