I’ve had to amputate arms and legs from many patients whose limbs could potentially have been saved if their infections had been diagnosed earlier. And these are the luckier ones—some patients don’t make it.
Eric R. Henderson, MDThe words “flesh-eating bacteria” may conjure images of a widespread infection leading to a zombie apocalypse in a sci-fi film. The reality is a lot less sensational, but no less deadly: mortality rates from necrotizing soft-tissue infections are as high as 30%, and often aren’t caught until it’s too late.
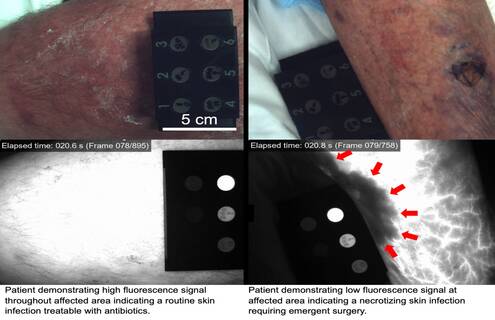
“Patients who have necrotizing infections usually present with skin changes that are indistinguishable from a routine skin infection,” said Eric R. Henderson, MD, an orthopaedic surgeon at Dartmouth Health’s Dartmouth Hitchcock Medical Center. “This is actually what makes these infections so dangerous. Because they don’t initially appear serious, diagnosis is often delayed, requiring more radical treatment that often includes amputation.”
Flesh-eating bacteria spreads quickly when it enters a particular tissue layer beneath the skin, and it can happen anywhere, like working or playing outside or swimming in the ocean. A lack of accurate diagnostic tools for the presence of flesh-eating bacteria has left physicians with few options to guide treatment for potentially affected patients.
Henderson recently led a first-in-kind study with colleagues from Dartmouth Health, Dartmouth College’s Geisel School of Medicine and Thayer School of Engineering, and other academic research institutions, using fluorescence to distinguish between routine skin infections and the more deadly necrotizing infections. Their findings were published in the Journal of Biomedical Optics.
Henderson and his co-investigators obtained a grant from the National Institute of Allergy and Infectious Diseases to study the use of fluorescent dye, injected intravenously, as a diagnostic tool for patients who present in the emergency department with a suspected necrotizing soft-tissue infection. The researchers hypothesized that there would be signal voids—dark areas in an MRI image that the dye doesn’t penetrate—in infected areas of the tissue. Of the 14 patients studied, all who did have necrotic tissue had prominent signal voids not visible to the naked eye.
“I’ve had to amputate arms and legs from many patients whose limbs could potentially have been saved if their infections had been diagnosed earlier. And these are the luckier ones—some patients don’t make it,” said Henderson, who plans to apply for another grant to study the use of fluorescence as a surgical guidance tool as well. “Flesh-eating bacteria infections are surprisingly easy to get and often have devastating impacts on patients and their loved ones. This research offers hope to physicians for an effective way of diagnosing these infections in order to reduce the need for radical surgery and improve survival.”
To read Henderson’s study, visit bit.ly/42J9RQd.
About Dartmouth Health
Dartmouth Health, New Hampshire’s only academic health system and the state’s largest private employer, serves patients across northern New England. Dartmouth Health provides access to more than 2,000 providers in almost every area of medicine, delivering care at its flagship hospital, Dartmouth Hitchcock Medical Center (DHMC) in Lebanon, NH, as well as across its wide network of hospitals, clinics and care facilities. DHMC is consistently named the #1 hospital in New Hampshire by U.S. News & World Report, and is recognized for high performance in numerous clinical specialties and procedures. Dartmouth Health includes Dartmouth Cancer Center, one of only 57 National Cancer Institute-designated Comprehensive Cancer Centers in the nation, and the only such center in northern New England; Dartmouth Health Children’s, which includes the state’s only children’s hospital and multiple locations around the region; member hospitals in Lebanon, Keene, Claremont and New London, NH, and Windsor and Bennington, VT; Visiting Nurse and Hospice for Vermont and New Hampshire; and more than 24 clinics that provide ambulatory and specialty services across New Hampshire and Vermont. Through its historical partnership with Dartmouth and the Geisel School of Medicine, Dartmouth Health trains nearly 400 medical residents and fellows annually, and performs cutting-edge research and clinical trials recognized across the globe with Geisel and the White River Junction VA Medical Center in White River Junction, VT. Dartmouth Health and its more than 13,000 employees are deeply committed to serving the healthcare needs of everyone in our communities, and to providing each of our patients with exceptional, personal care.